Treatment and Prevention of Bisphosphonate Induced Osteonecrosis of the Jaws
Treatment and Prevention of Bisphosphonate Induced Osteonecrosis of the Jaws
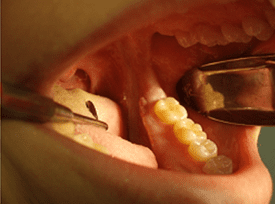
Figure 1, Area of exposed necrotic bone in the lingual gutter region of the mandible.
Bisphosphonates are therapeutic agents utilized in the treatment of osteoclast-mediated bone loss due to osteoporosis, hypercalcemia of malignancy, Paget’s disease of the bone, multiple myeloma, and metastatic malignancies such as breast, kidney, prostate and lung cancer (1,2,3). By far, the most common clinical condition treated with bisphosphonate therapy is osteoporosis. According to the National Osteoporosis Foundation, osteoporosis is a major public health threat for an estimated 44 million Americans, or 55 percent of the people 50 years of age or older.
Currently in the US, 10 million individuals are estimated to already have osteoporosis and approximately 34 million are estimated to have low bone mass, placing them at increased risk for osteoporosis and fractures. As the American population ages, so will the number of individuals at risk for osteoporosis and the number of individuals undergoing bisphosphonate therapy.
The first published report of bisphosphonate induced osteonecrosis of the jaw (BIONJ) was by Marx in September of 2003 (4). As of May 2007, more than 300 publications have linked bisphosphonates to osteonecrosis in the jaws and an estimated 10,000 individual cases have been reported (3). Bisphosphonates may be administered via oral or intravenous means. Oral bisphosphonates may be administered once per day, once per week or once per month. IV bisphosphonates may be administered monthly or even yearly in the case of the very potent Zometa.
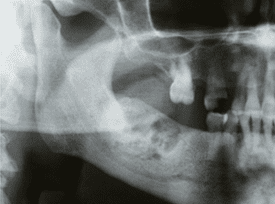
Figure 2, radiographic appearance of BIONJ in the posterior mandible.
Most authors believe the incidence of oral bisphosphonate-induced osteonecrosis to be approximately 0.015% after three years of oral therapy. The incidence of intravenous bisphosphonate-induced osteonecrosis is much higher than the oral form and has been reported to be as high as 30%. However, most studies report a more reliable incidence of intravenous bisphosphonate-induced osteonecrosis of approximately 8% (3).
BIONJ typically presents as areas of exposed bone in either the mandible or the maxilla (2:1 ratio of mandible to maxilla) that fails to heal despite local measures in a reasonable amount of time (8 weeks or greater) (1, 3, 5, 6). Patients may be asymptomatic or may complain of pain, drainage, foul taste, loose teeth or numbness (Figures 1, 3, 4). Radiographic evidence of BIONJ includes thickening or widening of the periodontal ligament space, areas of sclerotic bone and bone sequestrum formation and necrosis in the later stages (Figures 2, 5)(3,5).
The American Association of Oral and Maxillofacial Surgeons (AAOMS) consider patients to have BIONJ if the three following characteristics are present:
- Current or previous treatment with a bisphosphonate
- Exposed, necrotic bone in the maxillofacial region that has persisted for more than 8 weeks
No history of radiation therapy to the jaws (1)
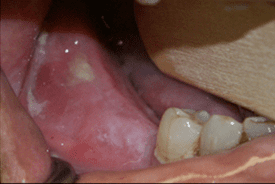
Figure 3, clinical presentation of BIONJ in the patient in Figure 2.
Bisphosphonates vary in their relative potencies, however, intravenous bisphosphonates are more potent than oral forms. Oral bisphosphonates tend to accumulate in the bone much slower than intravenous forms. As such, patients are at an increased risk of developing BIONJ after six months of intravenous bisphosphonates usage versus three years of oral bisphosphonate use (1, 3, 6, 7). Osteonecrosis associated with intravenous bisphosphonates is generally more invasive, associated with a poorer prognosis and less responsive to surgical debridement than BIONJ associated with oral bisphosphonate therapy (3).

Figure 4, area of exposed, necrotic bone in patient with BIONJ of left mandible.
Dental treatment of patients undergoing bisphosphonate therapy depends on the potency of the bisphosphonate and the length of treatment (1). In general, patients taking oral bisphosphonates for less than three years have little risk of developing BRONJ and can be treated as any other patient (3, 7). For patients with a history of three years or more of oral bisphosphonate therapy, patients should be informed that there is a small, but definite risk of developing BIONJ (1,5). As such, elective invasive procedures such as extractions, preprosthetic surgery and periodontal surgery may be performed after informed consent documenting the risk of BIONJ (5).
For patients with a history of 6 or more months of intravenous bisphosphonate usage, all invasive oral surgery procedures should be deferred unless no other treatment option exists. Teeth that are nonrestorable are best treated with root canal therapy and crown amputation, teeth with failing root canal therapy are best treated with retreats and mobile teeth are best treated with splinting. Noninvasive dental procedures such as crown and bridge, removable partial dentures, complete dentures, root canal therapy, supragingival scaling and dental prophylaxis should be performed at any time on patients undergoing bisphosphonate therapy in order to maintain dental health and eliminate the need for future invasive procedures (1, 3, 7).
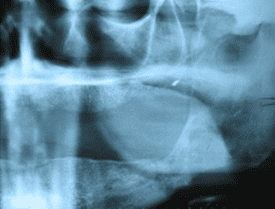
Figure 5, panorex of patient in Figure 4 with BIONJ to left posterior mandible.
Prior to the initiation of intravenous bisphosphonate therapy certain dental procedures should be done in order to minimize the occurrence of BIONJ. All teeth that are hopeless, nonrestorable, abscessed, failing root canal therapy and grossly periodontally involved should be extracted. Periodontal procedures should be performed in an attempt to arrest periodontal disease and create a healthier oral environment. Patients with full or partial dentures should be examined for areas of mucosal trauma, especially along the lingual flange area. Extensive patient education on oral hygiene and early signs of BIONJ are imperative (1, 3, 7).
With over 190 million prescriptions for bisphosphonates dispensed worldwide, prevention, early recognition and appropriate referral/treatment will help to minimize the late complications of bisphosphonate induced osteonecrosis of the jaw (BIONJ)(1, 5).
References:
- American Association Oral Maxillofacial Surgeons. Position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg 65(3): 369, 2007
- Drake MT, Clarke BL, Khosla S: Bisphosphonates: Mechanism of action and role in clinical practice. Mayo Clin Proc 83(9): 1032, 2008
- Sawatari Y, Marx RE: Bisphosphonate and bisphosphonate induced osteonecrosis. Oral Maxillofac Clin N Am 19(4): 487, 2007
- Marx RE: Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 61(9): 1115, 2003
- Bisphosphonate-related osteonecrosis of the jaw (BRONJ). AAOMS Surgical Update 20(2): 1, 2007
- Marx RE, Sawatari, Fortin M, et al: Bisphosphonate induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risks factors, recognition, prevention, and treatment. J Oral Maxillofac Surg 63(X): 1567, 2005
- Marx RE, Cillo JE, Ulloa JJ: Oral bisphosphonate induced osteonecrosis: risk factors, prediction of risk using serum CTX testing, prevention, and treatment. J Oral Maxillofac Surg 65: 2397, 2007
Other Considerations: Patients with certain repaired and congenital coronary heart disease (CHD), prosthetic heart valves, cardiac transplantation recipients whom have developed cardiac valvulopathy, previous infective endocarditis, artificial joints within the past 6 months and/or cardiac stents are subject to antibiotic prophylaxis 1 hour prior to your appointment.
